Treatment outcomes of Tuberculosis single infection and Tuberculosis/HIV co-infection in Rivers State University Teaching Hospital, Nigeria.
Main Article Content
Abstract
Introduction: Tuberculosis (TB) and TB/HIV co-infection are significant contributors to morbidity and mortality globally. The interaction between these two infections is multifaceted, with each disease influencing the epidemiology and progression of the other, which poses diagnostic and therapeutic challenges, particularly in developing countries. This study evaluated and compared the treatment outcomes of TB single infection and TB/HIV co-infection among patients at Rivers State University Teaching Hospital.
Methods: This was a two-year retrospective review of the clinical records of all adult patients with tuberculosis and TB/HIV coinfection at the tuberculosis clinic of RSUTH between January 2023 and December 2024. Patients’ clinical records were assessed to extract demographic data, retroviral status, treatment outcomes and analysed using SPSS version 27.
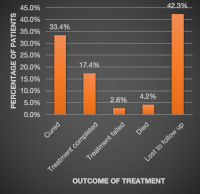
Results: A total of 685 adult patients were involved in the study; over half (52.0%) were aged between 21 and 40 years old. Mean (SD) = 34 (4.5), and 383 (55.9%) were male. Up to 33.6% were TB/HIV co-infected, with 216 persons on antiretroviral therapy. Patients with TB-only infections had significantly higher cure rates (37.8% 24.8%, p value = 0.001), while those with TB/HIV co-infection experienced higher mortality (9.6% vs. 1.5%, p value = 0.001) and were more lost to follow-up (49.5% vs. 38.6%, p value = 0.005).
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
How to Cite
References
Barberis I, Bragazzi NL, Galluzzo L, Martini M. The history of tuberculosis: from the first historical records to the isolation of Koch's bacillus. J Prev Med Hyg. 2017 Mar;58(1):E9-E12. PMID: 28515626; PMCID: PMC5432783
Global Tuberculosis Report 2024 [Internet]. [cited 2025 Mar 26]. Available from: https://www.who.int/teams/global-programme-on-tuberculosis-and-lung-health/tb-reports/global-tuberculosis-report-2024
Selimin DS, Ismail A, Ahmad N, Ismail R, Mohd Azman NF, Azman A. Tuberculosis Treatment Outcome in Patients with TB-HIV Coinfection in Kuala Lumpur, Malaysia. J Trop Med. 2021 May 29;2021:9923378. doi: 10.1155/2021/9923378. PMID: 34194511; PMCID: PMC8181108.
Tola A, Mishore KM, Ayele Y, Mekuria AN, Legese N. Treatment Outcome of Tuberculosis and Associated Factors among TB-HIV Co-Infected Patients at Public Hospitals of Harar Town, Eastern Ethiopia. A five-year retrospective study. BMC Public Health. 2019 Dec 10;19(1):1658. doi: 10.1186/s12889-019-7980-x. PMID: 31822286; PMCID: PMC6902430.
Torpey K, Agyei-Nkansah A, Ogyiri L, Forson A, Lartey M, Ampofo W, Akamah J, Puplampu P. Management of TB/HIV co-infection: the state of the evidence. Ghana Med J. 2020 Sep;54(3):186-196. doi: 10.4314/gmj.v54i3.10. PMID: 33883764; PMCID: PMC8042796.
Global HIV Programme [Internet]. [cited 2025 Mar 26]. Available from: https://www.who.int/teams/global-hiv-hepatitis-and-stis-programmes/hiv/treatment/tuberculosis-hiv
HIV and Tuberculosis. World Health Organisation [Internet]. [cited 2025 Mar 26]. Available from: https://www.who.int/westernpacific/health-topics/hiv-aids/hiv-and-tuberculosis
Sullivan A, Nathavitharana RR. Addressing TB-related mortality in adults living with HIV: a review of the challenges and potential solutions. Ther Adv Infect Dis. 2022 Mar 18;9:20499361221084163. doi: 10.1177/20499361221084163. PMID: 35321342; PMCID: PMC8935406.
Cohen A, Mathiasen VD, Schön T, Wejse C. The global prevalence of latent tuberculosis: a systematic review and meta-analysis. Eur Respir J. 2019 Sep 12;54(3):1900655. doi: 10.1183/13993003.00655-2019. PMID: 31221810.
Parker E, Judge MA, Macete E, Nhampossa T, Dorward J, Langa DC, Schacht C, Couto A, Vaz P, Vitoria M, Molfino L, Idowu RT, Bhatt N, Naniche D, Le Souëf PN. HIV infection in Eastern and Southern Africa: Highest burden, largest challenges, greatest potential. South Afr J HIV Med. 2021 May 28;22(1):1237. doi: 10.4102/sajhivmed.v22i1.1237. PMID: 34192070; PMCID: PMC8182467.
TUBERCULOSIS PREVENTIVE THERAPY SURGE PLAN AND ROADMAP, 2022 | NTBLCP | National Tuberculosis & Leprosy Control Programme [Internet]. [cited 2025 Mar 26]. Available from: https://ntblcp.org.ng/resources/tuberculosis-preventive-therapy-surge-plan-and-roadmap-2022/
Sinshaw Y, Alemu S, Fekadu A, Gizachew M. Successful TB treatment outcome and its associated factors among TB/HIV co-infected patients attending Gondar University Referral Hospital, Northwest Ethiopia: an institution based cross-sectional study. BMC Infect Dis. 2017 Feb 8;17(1):132. doi: 10.1186/s12879-017-2238-7. PMID: 28178936; PMCID: PMC5299781.
Abere Sarah, Dan-Jumbo Alali, Oyan Boma, Eno Gomba, Bawo Michael, Asonye Samuel and Alabi Ajibola. Same Day Antiretroviral Therapy Initiation, Prevalence and Co-factors of Advanced HIV Disease in an African Population- A 1 Year Report. International STD Research and Reviews, 2022; 11(2): 47-56
Bruchfeld J, Correia-Neves M, Källenius G. Tuberculosis and HIV Coinfection. Cold Spring Harb Perspect Med. 2015 Feb 26;5(7):a017871. doi: 10.1101/cshperspect.a017871. PMID: 25722472; PMCID: PMC4484961.
Pawlowski A, Jansson M, Sköld M, Rottenberg ME, Källenius G. Tuberculosis and HIV co-infection. PLoS Pathog. 2012 Feb;8(2):e1002464. doi: 10.1371/journal.ppat.1002464. Epub 2012 Feb 16. PMID: 22363214; PMCID: PMC3280977.
Nnenna Nnadi, Alali Dan-Jumbo, Boma Oyan and Sarah Abere. Level and elements of satisfaction among patients on Anti-retroviral therapy enrolled in differentiated care in south- south Nigeria. Greener Journal of Medical Sciences, 2023; 13(1): 61-68
World Health Organization. (2013). Definitions and reporting framework for tuberculosis – 2013 revision: updated December 2014 and January 2020. World Health Organization. https://iris.who.int/handle/10665/79199
Tuberculosis Key Facts. World Health Organisation. [Internet]. [cited 2025 Mar 26]. Available from: https://www.who.int/news-room/fact-sheets/detail/tuberculosis
Adepoju VA, Adelekan A, Etuk V, Onoh M, Olofinbiyi B. How Do Private Providers Unaffiliated With the Nigeria National TB Program Diagnose and Treat Drug-Susceptible TB Patients? A Cross-Sectional Study. Glob Health Sci Pract. 2022 Dec 21;10(6):e2200210. doi: 10.9745/GHSP-D-22-00210. PMID: 36951286; PMCID: PMC9771464.
Horton KC. Understanding sex disparities in tuberculosis and assessing the potential impact of strategies to improve men’s access to care (Doctoral dissertation, London School of Hygiene & Tropical Medicine).
Adamu AL, Gadanya MA, Abubakar IS, Jibo AM, Bello MM, Gajida AU, Babashani MM, Abubakar I. High mortality among tuberculosis patients on treatment in Nigeria: a retrospective cohort study. BMC Infect Dis. 2017 Feb 23;17(1):170. doi: 10.1186/s12879-017-2249-4. PMID: 28231851; PMCID: PMC5324260.
Horne DJ, Kohli M, Zifodya JS, Schiller I, Dendukuri N, Tollefson D, Schumacher SG, Ochodo EA, Pai M, Steingart KR. Xpert MTB/RIF and Xpert MTB/RIF Ultra for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane Database Syst Rev. 2019 Jun 7;6(6):CD009593. doi: 10.1002/14651858.CD009593.pub4. Update in: Cochrane Database Syst Rev. 2021 Feb 22;2:CD009593. doi: 10.1002/14651858.CD009593.pub5. PMID: 31173647; PMCID: PMC6555588.
Boehme CC, Nicol MP, Nabeta P, Michael JS, Gotuzzo E, Tahirli R, Gler MT, Blakemore R, Worodria W, Gray C, Huang L, Caceres T, Mehdiyev R, Raymond L, Whitelaw A, Sagadevan K, Alexander H, Albert H, Cobelens F, Cox H, Alland D, Perkins MD. Feasibility, diagnostic accuracy, and effectiveness of decentralised use of the Xpert MTB/RIF test for diagnosis of tuberculosis and multidrug resistance: a multicentre implementation study. Lancet. 2011 Apr 30;377(9776):1495-505. doi: 10.1016/S0140-6736(11)60438-8. Epub 2011 Apr 18. PMID: 21507477; PMCID: PMC3085933.
Chakaya J, Petersen E, Nantanda R, Mungai BN, Migliori GB, Amanullah F, Lungu P, Ntoumi F, Kumarasamy N, Maeurer M, Zumla A. The WHO Global Tuberculosis 2021 Report–not-so-good news and turning the tide back to End TB. Int J Infect Dis. 2022 doi: 10.1016/j.ijid.2022.03.011.
Danlami MB, Aliyu B, Samuel G. Incidence of rifampicin-resistance presumptive M. Tuberculosis cases among outpatients in Kebbi State, Nigeria. Afr J Infect Dis. 2021;15(1):47–52. doi: 10.21010/ajid.v15i1.6
Oladimeji O, Adepoju V, Anyiam FE, San JE, Odugbemi BA, Hyera FL, Sibiya MN, Yaya S, Zoakah AI, Lawson L. Treatment outcomes of drug-susceptible Tuberculosis in private health facilities in Lagos, South-West Nigeria. PLoS ONE. 2021;16(1):e0244581. doi: 10.1371/journal.pone.0244581
Pasipanodya, J.G., McNabb, S.J., Hilsenrath, P. et al. Pulmonary impairment after tuberculosis and its contribution to TB burden. BMC Public Health 10, 259 (2010). https://doi.org/10.1186/1471-2458-10-259
Suthar AB, Lawn SD, del Amo J, Getahun H, Dye C, Sculier D, Sterling TR, Chaisson RE, Williams BG, Harries AD, Granich RM. Antiretroviral therapy for prevention of tuberculosis in adults with HIV: a systematic review and meta-analysis. PLoS Med. 2012;9(7):e1001270. doi: 10.1371/journal.pmed.1001270. Epub 2012 Jul 24. PMID: 22911011; PMCID: PMC3404110.
Osei E, Oppong S, Adanfo D, Doepe BA, Owusu A, Kupour AG, Der J. Reflecting on tuberculosis case notification and treatment outcomes in the Volta region of Ghana: a retrospective pool analysis of a multicentre cohort from 2013 to 2017. Glob Health Res Policy. 2019 Dec 17;4:37. doi: 10.1186/s41256-019-0128-9. PMID: 31890895; PMCID: PMC6916450.
Kigozi G, Heunis C, Chikobvu P, Botha S, van Rensburg D. Factors influencing treatment default among tuberculosis patients in a high burden province of South Africa. Int J Infect Dis. 2017 Jan;54:95-102. doi: 10.1016/j.ijid.2016.11.407. Epub 2016 Nov 25. PMID: 27894985.
Nagu TJ, Aboud S, Mwiru R, Matee MI, Rao M, Fawzi WW, Zumla A, Maeurer MJ, Mugusi F. Tuberculosis associated mortality in a prospective cohort in Sub Saharan Africa: Association with HIV and antiretroviral therapy. Int J Infect Dis. 2017 Mar;56:39-44. doi: 10.1016/j.ijid.2017.01.023. Epub 2017 Feb 1. PMID: 28161460.