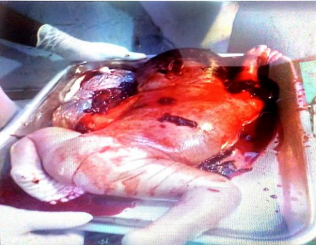
Spontaneous Rupture of an Unscarred Multigravid Uterus: A Case Report
Main Article Content
Abstract
Introduction: Uterine rupture during pregnancy is a life-threatening condition that is associated with high maternal or foetal mortality. Maternal morbidity and mortality have been a major World Health Organization concern over the years, especially in sub-Saharan Africa, of which Nigeria is not exempt.
Method: This paper reports a case of uterine rupture with hypovolemic shock in an unscarred uterus. A previous scarred uterus is the commonest risk factor for uterine rupture. Spontaneous rupture is a rare occurrence.
Result: The patient was an unbooked 41‑year‑old gravida 5, para 4 + 0 (4 alive) at an estimated gestational age of 39 weeks + 4 days. The case was managed at our facility following a referral from a primary health centre in Abeokuta. She was referred on account of acute abdominal pain and signs and symptoms of haemorrhagic shock while
in labour.
Conclusion: The foetal heart rate could not be heard with the handheld Doppler and bedside ultrasound scans. A suspicion of uterine rupture, complicated by hypovolemic shock and intrauterine foetal death, was entertained. She had uterine repair and bilateral tubal ligation. Severe anaemia was corrected with appropriate pints of blood.
Postpartum period was uneventful.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
How to Cite
References
Omole-Ohonsi A, Attah R. Risk Factors for Ruptured Uterus in a Developing Country. Gynecol Obstetric 2011, 1:1. DOI: 10.4172/2161-0932.1000102.
Berhe Y, Wall LL. Uterine rupture in resource-poor countries. Obstet. Gynecol. Surv. 2014; 69 (11): 695-707.
Astatikie G, Limenih MA, Kebede M. Maternal and foetal outcomes of uterine rupture and factors associated with maternal death secondary to uterine rupture. BMC Pregnancy Childbirth. 2017;17(1):117. doi.org/10.1186/s12884-017-1302-z
Saghafi N, Maleki A, Ayati S, Shirinzadeh L. First trimester uterine rupture, a rare but life-threatening event: a case report. Iran J Med Sci. 2019;44(5):422–426.
Motomura K, Ganchimeg T, Nagata C, Ota E, Vogel JP, Betran AP, et al. Incidence and outcomes of uterine rupture among women with prior caesarean section: WHO Multicountry Survey on Maternal and Newborn Health. Scientific reports. 2017 M;7(1):44093. doi: 10.1038/srep44093.
Wan S, Yang M, Pei J, Zhao X, Zhou C, Wu Y, et al. Pregnancy outcomes and associated factors for uterine rupture: an 8-year population-based retrospective study. BMC Pregnancy Childbirth. 2022; 22(1): 91. https://doi.org/10.1186/s12884-022-04415-6
Nonye-Enyidah EI, Esiogu LF, Esiogu B, Amadi S, Wekere C, Mba A. Uterine Rupture: Prevalence and Risk Factors at a Tertiary Institution in Nigeria. Asian J Pregnancy Childbirth. 2025 Feb 10;8(1):24-33.
Desta M, Kassa GM, Getaneh T, Sharew Y, Alemu AA, Birhanu MY, Yeneabat T, Alamneh YM, Amha H. Maternal and perinatal mortality and morbidity of uterine rupture and its association with prolonged duration of operation in Ethiopia: A systematic review and meta-analysis. PloS one. 2021;16(4):e0245977.
Mutiso SK, Oindi FM, Mundia DM. Uterine rupture in the first trimester: a case report and review of the literature. J Med Case Rep. 2024;18(1):1-6.
Pinton A, Boudier E, Joal A, Sananes N, Severac F, Langer B, et al. Risk factors and clinical presentation of uterine rupture in the unscarred uterus: a case-control study. J. Pregnancy Child Health. 2016;3(5):1-6.
Abrar S, Abrar T, Sayyed E, Naqvi SA. Ruptured uterus: Frequency, risk factors and feto-maternal outcome: Current scenario in a low-resource setup. Plos one. 2022;17(4): e0266062. https://doi.org/10.1371/journal.pone.0266062
Desseauve D, Bonifazi-Grenouilleau M, Fritel X, Lathélize J, Sarreau M, Pierre F. Foetal heart rate abnormalities associated with uterine rupture: a case–control study: A new time-lapse approach using a standardised classification. Eur J Obstet Gynecol Reprod Biol. 2016; 197:16-21.
Yalla A, Vaddadi S. Spontaneous uterine rupture of an unscarred uterus before labour—a case report. Indian J Obstet and Gynecol Res. 2017;4(3):306-308.
14. Li Y, Tian Y, Liu N, Chen Y, Wu F. Analysis of 62 placental abruption cases: risk factors and clinical outcomes. Taiwanese J Obstet Gynecol. 2019;58(2):223–226. doi: 10.1016/j.tjog.2019.01.010.
Aboughalia H, Basavalingu D, Revzin MV, Sienas LE, Katz DS, Moshiri M. Imaging evaluation of uterine perforation and rupture. Abdom. Radiol. 2021;46(10):4946-4966.
Segal R, Levin I, Many A, Michaan N, Laskov I, Amikam U, et al. Laparoscopic management of suspected postpartum uterine rupture: a novel approach. The J Matern Fetal Neonatal Med. 2022;35(25):9362-9367.
Pecorella G, Licchelli M, Panese G, Morciano A, Sparic R, Kosmas I, et al. Laparoscopic repair of uterine rupture after delivery: A comprehensive evaluation of the uterine rupture management, with a proposal for a surgical method. Int J Gynecol Obstet. 2025;170(2):551-560.
Al-Zirqi I, Daltveit AK, Vangen S. Infant outcome after complete uterine rupture. Am J Obstet Gynecol. 2018; 219(1): e1-e109.
Shao L, Yang Z, Yan H, Xu R. Uterine rupture in patients with a history of hysteroscopy procedures: Case series and review of literature. Medicine. 2024;103(10):e37428. doi: 10.1097/MD.0000000000037428
You SH, Chang YL, Yen CF. Rupture of the scarred and unscarred gravid uterus: Outcomes and risk factors analysis. Taiwanese J Obstet Gynecol. 2018;57(2):248-254.