Awareness and Perceived Availability of Emergency Transport Schemes for Maternal Health in Kaduna State, Nigeria
Main Article Content
Abstract
Introduction: Timely access to skilled care during pregnancy and childbirth is key to reducing maternal deaths. The Emergency Transport Scheme (ETS) was introduced in Kaduna State to address the second delay in accessing skilled care. This study assessed awareness and perceived availability of ETS services among pregnant women in Kaduna State, Nigeria.
Methods: A community-based, cross-sectional study using a mixed-methods approach was conducted in December 2019 among 309 women of reproductive age who had been pregnant in the year preceding the study. A multistage sampling technique was used to select respondents across three Local Government Areas (LGAs) representing the three senatorial zones of the state. Quantitative data were collected using interviewer-administered questionnaires and analysed. Descriptive and bivariate analyses were conducted. Qualitative data from focus group discussions and key informant interviews were analysed thematically.
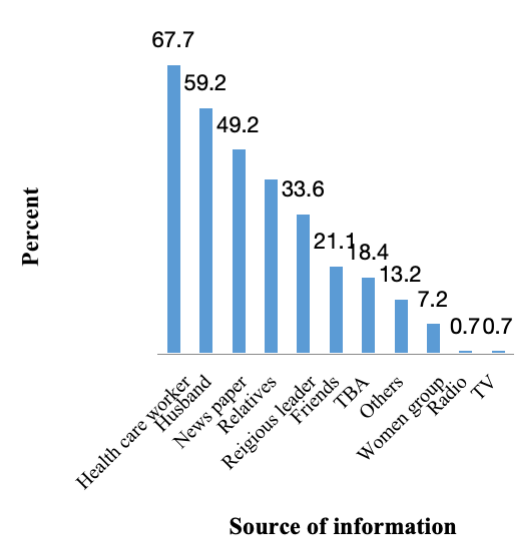
Results: Overall, 49.2% of respondents were aware of ETS services. Health workers (44.7%) were the main source of information. Only 36.1% perceived ETS to be readily available when needed. ETS awareness was significantly associated with respondents’ education level (p < 0.001), ANC attendance (p < 0.001), and LGA of residence (p = 0.027). The qualitative findings from this research revealed limited awareness of ETS in the community and irregular availability of the scheme.
Conclusion: Nearly half of the participants were aware of ETS services, but the perceived availability was low. Improving sensitisation, strengthening community engagement and addressing gaps in logistics have the potential of enhancing the utilisation of ETS services.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
How to Cite
References
World Health Organization. Trends in maternal mortality 2000 to 2020: estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. Geneva: WHO; 2023.
National Population Commission (NPC) [Nigeria], ICF. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, MD, USA: NPC and ICF; 2019.
Ibrahim UM, Shehu AU, Jiya NM, Abubakar A, Bashir IM. Knowledge and utilization of Emergency Transport Scheme among women in Zaria, Kaduna State. J Community Med Prim Health Care. 2020;32(2):23–32.
Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38(8):1091–110.
Fagbamigbe AF, Idemudia ES. Barriers to antenatal care use in Nigeria: Evidence from non-users and implications for maternal health programming. BMC Pregnancy Childbirth. 2015;15:95.
Doctor HV, Findley SE, Ager A, Cometto G, Afenyadu GY. Using community-based research to shape the design and delivery of maternal health services in Northern Nigeria. Reprod Health Matters. 2012;20(39):104–12.
Abubakar IS, Adamu AN, Adamu H. Determinants of maternal healthcare utilization in Kano rural communities. Niger J Med. 2019;28(3):271–6.
Adegoke AA, Mani S, Abubakar A, Van den Broek N. Community perceptions of the Emergency Transport Scheme in rural Northern Nigeria. PLoS One. 2020;15(12):e0244092.
Society for Family Health (SFH). Evaluation Report: Emergency Transport Scheme implementation in Nigeria. Abuja: SFH; 2020.
National Primary Health Care Development Agency (NPHCDA). ETS Monitoring Report: Challenges and Best Practices. Abuja: NPHCDA; 2021.
Babalola S, Fatusi A. Determinants of use of maternal health services in Nigeria – Looking beyond individual and household factors. BMC Pregnancy Childbirth. 2009;9:43.
Federal Ministry of Health (FMOH). National Strategic Health Development Plan II (2018–2022). Abuja: FMOH; 2018.
Barber C, Clark S. Review of the emergency transport scheme and community health volunteer mobility initiatives in Madagascar, under the MAHEFA programme. Transaid; 2016. p. 20–29. Available from: http://www.transaid.org
Ahmed S, Creanga AA, Gillespie DG, Tsui AO. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS One. 2010;5(6): e11190.
Okonofua FE, Ntoimo LF, Ogu RN, Galadanci HS, Gana M, Okike ON, Abdus-Salam RA, Adeoye IA, Abe E, Adegoke KK, Oyeneyin LO, Gbolahan OB. Association of the availability of emergency obstetric care services with maternal mortality in northern Nigeria: a hospital-based study. BMC Health Serv Res. 2022;22(1):50.
Mattson J. Transportation, distance, and health care utilization for older adults in rural and small urban areas. Transp Res Rec. 2011;(2265):192–9. Available from: https://trrjournalonline.trb.org/doi/abs/10.3141/2265-22
Aldrich E. Transport-related delays and maternal mortality in Uganda: the effects of managed and controlled mobility on maternal health and well-being [dissertation]. Utrecht: Utrecht University; 2014. Available from: https://dspace.library.uu.nl/handle/1874/297356
Shobo O. Access to safe emergency obstetric care using volunteer public transport workers in Nigeria: Approach, results and challenges. Presented at: American Public Health Association Conference (APHA); 2014.
Cochran WG. Sampling Techniques. New York, London: John Wiley and Sons; 1963. https://doi.org/10.1002/bimj.19650070312
Adegoke AA, Mani S, Abubakar A, Van den Broek N. Community perceptions of the Emergency Transport Scheme in rural Northern Nigeria. PLoS One. 2020;15(12): e0244092.
Magnani R. Sampling Guide. Washington (DC): Food and Nutrition Technical Assistance Project (FANTA); 1999. Available from: https://www.fantaproject.org/sites/default/files/resources/Sampling-Guide-Aug2000.pdf
Fagbamigbe AF, Idemudia ES. Barriers to antenatal care use in Nigeria: Evidence from non-users and implications for maternal health programming. BMC Pregnancy Childbirth. 2015;15:95. Available from: https://www.ncbi.nlm.nih.gov/pubmed/25885481
Adedokun ST, Uthman OA, Adekanmbi VT. Awareness and use of maternal health services in Nigeria: Evidence from Gombe. African Journal of Reproductive Health. 2021;25(4):12–20. Available from: https://www.ajrh.info/index.php/ajrh/article/view/2813