Utilization of Antenatal Care and Delivery Services in Oyigbo Comprehensive Health Centre: A One-Year Review
Main Article Content
Abstract
Introduction: This study assessed the utilisation of antenatal care (ANC) and delivery services as well as factors influencing birth outcomes at the Oyigbo Comprehensive Primary Health Centre (OCPHC) in Rivers State, Nigeria.
Methods: A cross-sectional retrospective review was conducted on the records of 498 women aged 15–49 who accessed maternal services in 2024. Data were extracted using Kobo Toolbox Android devices and analysed with SPSS version 27, employing Pearson’s chi-square test for statistical associations.
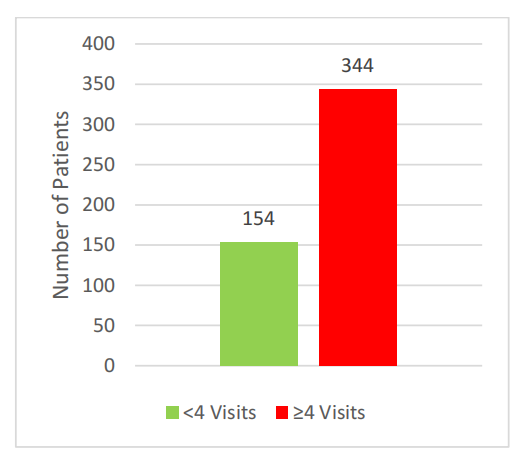
Results: The mean age of participants was 29.3 ± 5.4 years. Of the 498 women registered for ANC, 344 (69.1%) attended at least four ANC visits, indicating relatively high ANC utilisation. However, only 136 out of 464 recorded deliveries (29.3%) occurred at OCPHC, revealing a substantial gap between ANC attendance and facility-based delivery. Significant factors associated with delivering at OCPHC included the number of ANC visits and hepatitis status. A higher proportion of women who attended more ANC visits (4–6 visits: 34.1%; 7–9 visits: 55.8%) delivered at OCPHC (χ² = 79.55; p < 0.001). Additionally, 75% of hepatitis-positive women delivered at the facility (χ² = 8.56; p < 0.003). Maternal weight at booking also showed a significant association with birth outcomes.
Conclusion: The findings highlight the need to bridge the gap between ANC attendance and institutional delivery through enhanced health education and behavioural change strategies tailored to the local context.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
How to Cite
References
Citaristi I. United Nations Population Fund—UNFPA. In: The Europa Directory of International Organizations 2022 [Internet]. Routledge; 2022 [cited 2025 Jun 22]. p. 293–6. Available from: https://www.taylorfrancis.com/chapters/edit/10.4324/9781003292548-59/united-nations-population-fund%E2%80%94unfpa-ileana-citaristi
Otundo Richard M. WHO recommendations on antenatal care for a positive pregnancy experience in Kenya. Available SSRN 3449460 [Internet]. 2019 [cited 2025 Jun 22]; Available from: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3449460
Banke-Thomas A, Avoka CK on, Gwacham-Anisiobi U, Omololu O, Balogun M, Wright K, et al. Travel of pregnant women in emergency situations to hospital and maternal mortality in Lagos, Nigeria: a retrospective cohort study. BMJ Glob Health. 2022;7(4): e008604.
Trends in maternal mortality estimates 2000 to 2023. estimates WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division - Google Search [Internet]. [cited 2025 Aug 26]. Available from: https://www.who.int/publications/i/item/9789240108462
Dogbanya G. Maternal Mortality in Nigeria: Holding the Line in Uncertain Times. Ann Glob Health. 2025 Mar 25;91(1):16.
NPC, ICF. Nigeria Demographic and Health Survey 2023 – 24 Key Indicators Report. Abuja, Nigeria; 2023 p. 1–88.
Ossai EN, Eze II, Eke PC, Onah CK, Agu C, Ogbonnaya LU. Where, why and who delivers our babies? Examining the perspectives of women on utilization of antenatal and delivery services in a developing country. BMC Pregnancy Childbirth. 2023 Jan 2;23(1):1.
Tura G, Fantahun M, Worku A. The effect of health facility delivery on neonatal mortality: systematic review and meta-analysis. BMC Pregnancy Childbirth. 2013 Dec;13(1):18.
Oshinyemi TE, Aluko JO, Oluwatosin OA. Focused on antenatal care: Re-appraisal of current practices. Int J Nurs Midwifery. 2018;10(8):90–8.
Fagbamigbe AF, Olaseinde O, Fagbamigbe OS. Timing of first antenatal care contact, its associated factors and state-level analysis in Nigeria: a cross-sectional assessment of compliance with the WHO guidelines. BMJ Open. 2021 Sep;11(9):e047835.
Izuka E, Obiora-Izuka C, Asimadu E, Enebe J, Onyeabochukwu A, Nwagha U. Effect of Late Antenatal Booking on Maternal Anemia and Fetus Birth Weight on Parturients in Enugu, Nigeria: An Analytical Cross-Sectional Study. Niger J Clin Pract. 2023 May;26(5):558–65.
Ngxongo TSP. Basic Antenatal Care Approach to Antenatal Care. Sel Top Midwifery Care. 2019;1.
Organization WH. Births attended by skilled health personnel. Glob Health Obs Httpswww Who Intdataghodataindicatorsindicator-DetailsGHObirths-Attend--Skilled-Health-Pers--. 2021;
Abubakar S, Adamu D, Hamza R, Galadima JB. Determinants of home delivery among women attending antenatal care in Bagwai Town, Kano Nigeria. Afr J Reprod Health. 2017;21(4):73–9.
Johnson OE, Obidike PC, Eroh MU, Okpon AA, Bassey EI, Patrick PC, et al. Choices and determinants of delivery location among mothers attending a primary health facility in Southern Nigeria. Niger Postgrad Med J. 2020;27(1):42–8.
Triumph NA, Onyebuchi OB. Evaluation of antenatal care utilization studies in Nigeria from 1990-2020: A narrative review. J Clin Images Med Case Rep. 2021;2(6):1509.
He Q, Abdureyim M, He Z, Ma X, Huang M, Zhang T, et al. Factors associated with age-specific maternal health-seeking behaviours among women: A Multiple Indicator Cluster Survey-based study in 10 African countries. J Glob Health. 2022 Nov 8;12:04095.
Paul P, Chouhan P. Socio-demographic factors influencing utilization of maternal health care services in India. Clin Epidemiol Glob Health. 2020 Sep;8(3):666–70.
Oshun PO, Sunmonu OB. Prevalence of syphilis and associated risk factors among human immunodeficiency virus-infected patients at the Lagos University Teaching Hospital Nigeria: A cross-sectional study. J Clin Sci. 2024 Apr;21(2):88–92.
Olakunde BO, Adeyinka DA, Ndukwe CD, Oladele TT, Yahaya HB, Ijaodola OA. Antenatal hepatitis B screening in Nigeria: A comparative analysis with syphilis and HIV. Int J STD AIDS. 2021 Dec;32(14):1290–7.
Agu U, Agu MC, Nnaji GA. Utilisation of antenatal services at comprehensive health center umunya, anambra state: a retrospective study. Habert Open Access J [Internet]. 2015 [cited 2025 Apr 26]; Available from: https://www.academia.edu/download/116588892/2056-5690-2-2.pdf
Osungbade KO, Shaahu VN, Uchendu OC. Clinical Audit of Antenatal Service Provision in Nigeria. Health Care Women Int. 2011 Apr 11;32(5):441–52.
Imo CK. Influence of women’s decision-making autonomy on antenatal care utilisation and institutional delivery services in Nigeria: evidence from the Nigeria Demographic and Health Survey 2018. BMC Pregnancy Childbirth. 2022 Dec;22(1):141.
Kibria GMA, Shawon MSR, Nurunnabi M, Hasan MZ. The Relationship of Socioeconomic Status, Antenatal Care Visits, and Hospital Delivery in Bangladesh: Analysis of Demographic and Health Survey 2022. medRxiv. 2025;2025–03.
Nigusie A, Azale T, Yitayal M, Derseh L. Institutional delivery and associated factors in rural communities of Central Gondar Zone, Northwest Ethiopia. Ortega JA, editor. PLOS ONE. 2021 Jul 22;16(7):e0255079.
Green, E. C., Murphy, E. M., & Gryboski, K. (2020). The Health Belief Model. In K. Sweeny, M. L. Robbins, & L. M. Cohen (Eds.), The Wiley Encyclopedia of Health Psychology (pp. 211-214). John Wiley & Sons. - References - Scientific Research Publishing [Internet]. [cited 2025 Aug 26]. Available from: https://www.scirp.org/reference/referencespapers?referenceid=3581174
Shehu AY, Ogboghodo EO, Enaruna N, Jamda MA. Outcome of Delivery among HIV-Positive Women that Attended the Antenatal Clinic at the University of Benin Teaching Hospital, Benin City, Nigeria. Niger J Med. 2022 Mar;31(2):212–5.
Akselsson A, Rossen J, Storck-Lindholm E, Rådestad I. Prolonged pregnancy and stillbirth among women with overweight or obesity – a population-based study in Sweden including 64,632 women. BMC Pregnancy Childbirth. 2023 Jan 12;23(1):21.
Aune D, Saugstad OD, Henriksen T, Tonstad S. Maternal Body Mass Index and the Risk of Fetal Death, Stillbirth, and Infant Death: A Systematic Review and Meta-analysis. JAMA. 2014 Apr 16;311(15):1536.
Akpan UB, Akpanika C, Okpebri KO, Udeke U, Etuk SJ. The Prevalence of Maternal Obesity at First Antenatal Visit and Pregnancy Outcomes: A Prospective Cohort Study in a Southern Nigerian Region. Niger J Med. 2023 Sep;32(5):495–500.
Iyoke C, Ezugwu F, Ugwu, Lawani O, Onyebuchi AK. Retrospective cohort study of the effects of obesity in early pregnancy on maternal weight gain and obstetric outcomes in an obstetric population in Africa. Int J Womens Health. 2013 Aug;501.
Senbanjo OC, Akinlusi FM, Ottun TA. Early pregnancy body mass index, gestational weight gain and perinatal outcome in an obstetric population in Lagos, Nigeria. Pan Afr Med J. 2021;39:136.
Odar Stough C, Bolling C, Zion C, Stark LJ. Comparison of High and Normal Birth Weight Infants on Eating, Feeding Practices, and Subsequent Weight. Matern Child Health J. 2018 Dec;22(12):1805–14.
WHO. Low birth weight [Internet]. [cited 2025 Apr 26]. Available from: https://www.who.int/data/nutrition/nlis/info/low-birth-weight
Adhikary A, Begum A, Joty FS, Sarker NR, Akhter T. Pregnancy Outcome between Booked and Unbooked Cases in A Tertiary Level Hospital. J Shaheed Suhrawardy Med Coll. 2018 Jul 5;9(2):43–8.